Understanding Methylation: Why Your Body Might Be Struggling (And What Actually Helps)
Sarah came to see me completely exhausted.
Not just tired – that bone-deep fatigue where even simple tasks feel overwhelming. Her brain fog was so bad she’d forget what she was saying mid-sentence. She described it as just feeling “yuk” all the time, and nothing seemed to help.
We ran MTHFR genetic testing, and there it was: significant gene variants affecting her methylation cycle. Once we switched her to methylated B vitamins in the right forms and doses, things started shifting. Within 3-4 weeks, her energy improved noticeably. The brain fog lifted. She stopped feeling constantly “yuk.”
Here’s the thing about methylation: when it’s not working well, it affects almost everything. Mood, energy, detoxification, hormone metabolism, even how your DNA repairs itself. And the standard approach, just throw any old B vitamins at it – often misses the mark entirely.
What Actually Is Methylation (Without the Biochemistry Lecture)
Methylation is a biochemical process where your body adds small molecules called methyl groups (one carbon atom with three hydrogens) onto other molecules. Think of it like a tagging system – these methyl tags tell your body what to do with different molecules.
Those tags control hundreds of essential processes: turning genes on and off, making neurotransmitters, metabolizing hormones, detoxifying substances, even repairing DNA. The methyl groups get passed around like currency – donated from one molecule to another to keep these vital reactions running.
When methylation works well, you probably don’t notice it. When it doesn’t, you feel it everywhere:
- Persistent fatigue that sleep doesn’t fix
- Brain fog and poor concentration
- Mood issues – anxiety and depression are common
- Sensitivity to stress (you just can’t cope the way you used to)
- Hormone imbalances
- Poor detoxification (you react to everything)
- Slow healing and recovery
In my practice, people with methylation issues rarely have just one symptom. It’s usually a cluster: fatigue AND brain fog AND poor stress tolerance all together. That pattern is what makes me think about methylation support.
The MTHFR Gene: Should You Test or Not?
You’ve probably heard about MTHFR – it stands for methylenetetrahydrofolate reductase, which is exactly why everyone just says MTHFR. This gene produces an enzyme that’s critical for methylation, specifically for converting folate into its active form.
About 40-60% of the population has at least one MTHFR gene variant. The two most studied are C677T and A1298C. Having these variants doesn’t mean your methylation is definitely impaired – genetics is never that simple.
Here’s what matters: your genes are like a blueprint, but epigenetics determines whether those genes actually express. Your diet, stress levels, toxin exposure, gut health, and lifestyle all influence whether your MTHFR variants actually cause problems. This is why some people with the gene variants feel terrible while others feel fine.
Having MTHFR variants does mean you might need more nutritional support – particularly if your environment and lifestyle are stressing your system. But it’s not a life sentence. The right diet and targeted supplementation can often compensate entirely for the genetic weakness.
The Case for Testing
Genetic testing for MTHFR can be valuable if:
- Multiple family members have similar unexplained symptoms
- You’ve had pregnancy complications or multiple miscarriages
- You have a personal or family history of cardiovascular issues
- Standard B vitamin supplementation hasn’t helped (or made things worse)
- You want to understand your specific genetic picture
The testing itself is straightforward, usually a cheek swab, and the results don’t change. Your genes are your genes. What does change is our understanding of how to support them.
The Case for Not Testing
Here’s my honest take: you don’t always need the test. Sometimes the clinical picture is clear enough, and the treatment approach is similar whether you have confirmed MTHFR variants or not.
I see people get too caught up in their genetic results, almost using them as an identity. “I’m MTHFR” becomes their explanation for everything. But genetics is just one piece. Environmental factors, gut health, stress levels, and nutrient status often matter more than the gene variants themselves.
You might skip testing if:
- You’re on a tight budget and would rather invest in quality supplements
- The testing would create more anxiety than clarity
- You’re willing to try targeted support and see how you respond
- Your symptoms clearly improve with methylation support
The research here is nuanced. Having MTHFR variants increases risk for certain conditions, but it’s not deterministic. I’ve seen people with double variants (homozygous) who feel great, and people with no variants who struggle terribly. Context matters.
The Practical Approach: Start With Quality B Complexes
In my practice, I rarely prescribe individual B vitamins for methylation support. Most people do better with a quality B complex that contains all the B vitamins in their active, methylated forms or a B12 + Folate combo. B Vitamins work together as a team.
Why B complexes work better:
- The B vitamins support each other’s function
- You get proper ratios without having to figure out individual dosing
- Less risk of creating imbalances
- More convenient (one supplement instead of five)
The key is making sure your B complex contains the right forms – methylfolate (5-MTHF), methylcobalamin, and P5P, the active forms your body can use immediately without conversion.
Practitioner-grade supplements use these active forms. Cheap supermarket brands usually don’t.
Folate and B12: The Core Duo
These two are the stars of methylation support. Here’s where it gets tricky: synthetic folic acid (in most cheap supplements and fortified foods) needs to be converted to 5-MTHF (methylfolate) before your body can use it. If your MTHFR enzyme isn’t working efficiently, you get a traffic jam.
The solution? Skip the conversion step entirely. Use supplements that already contain 5-MTHF.
Look for: Methylfolate as 5-MTHF or L-methylfolate (not folic acid).
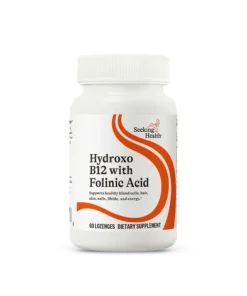
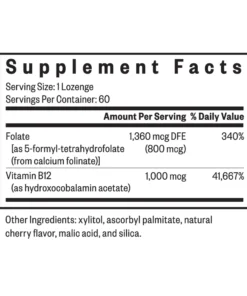
Similarly, most B12 supplements contain cyanocobalamin – a synthetic form your body has to convert. For methylation support, you want methylcobalamin or adenosylcobalamin. These are the active forms your cells can use directly.
Look for: Methylcobalamin or adenosylcobalamin (not cyanocobalamin).
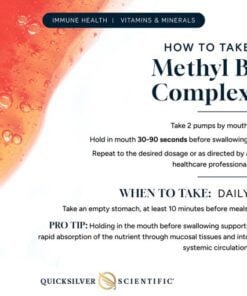
For people who need higher doses or prefer a targeted approach, sublingual methylcobalamin provides direct absorption, bypassing potential gut issues.
A pattern I’ve noticed: people often feel worse before better when they start methylated B12. This usually means methyl groups are suddenly available and your body is playing catch-up on all the processes it couldn’t complete before. It typically settles within 1-2 weeks.
Alternative Pathways: TMG (Betaine)
When your main folate pathway is sluggish, alternative pathways become important. TMG (trimethylglycine, also called betaine) donates methyl groups through a different route, taking pressure off the MTHFR-dependent pathway.
Look for: Trimethylglycine (TMG) or betaine, ideally combined with methylated B vitamins and riboflavin-5-phosphate.
Formulas that combine TMG with methylated B vitamins and riboflavin provide all the key nutrients working together. This is particularly useful for people with elevated homocysteine or those who don’t tolerate high-dose methylfolate well.
Dietary betaine from beetroot is valuable too, but you’d need to eat a lot of beetroot to match supplement doses.
Choline: The Often-Forgotten Methyl Donor
Choline provides another alternative methylation pathway. Eggs are the best food source (particularly the yolks), but supplementation can be helpful, especially for people who are plant-based or don’t eat eggs regularly.
Choline supplements support methylation through an alternative pathway while also providing benefits for mood and cellular signaling.
The Supporting Cast: Minerals Matter
B vitamins can’t do their job without adequate minerals. Magnesium and zinc are co-factors that dozens of methylation enzymes require. Most people are low in magnesium anyway – stress depletes it rapidly.
Start Low and Slow
This is critical. High-dose methylated B vitamins can make people feel awful – anxious, wired, irritable. Why? Because you’re suddenly flooding your system with methyl groups it hasn’t had access to for years.
Start with lower doses than recommended on the bottle. After 1-2 weeks, assess. If you feel good, you can gradually increase. If you feel worse, drop back down or take a break.
Some people feel dramatically better within days. Others need 4-6 weeks to notice changes. And a small group of people feel worse with standard methylation support – this might mean you’re an overmethylator or have other issues at play.
If you feel consistently worse (not just the temporary adjustment period), stop and reassess. Sometimes less is more, or you need a different approach entirely.
Diet: The Foundation That Supplements Can’t Replace
Before you rush to buy supplements, look at your diet. Methylation support starts in the kitchen.
Foods That Support Methylation:
Folate-rich foods:
- Dark leafy greens (spinach, kale, rocket)
- Lentils and legumes
- Asparagus
- Brussels sprouts
- Broccoli
- Liver (if you can stomach it – it’s genuinely one of the best sources)
Natural folate from food is different from synthetic folic acid. Your body handles it better, and there’s no risk of buildup.
Choline sources:
- Eggs (particularly the yolks)
- Liver and organ meats
- Fish and shellfish
- Chicken and turkey
- Cruciferous vegetables
B12 sources:
- Animal proteins (beef, lamb, fish)
- Shellfish
- Eggs
- Dairy products
If you’re plant-based, B12 supplementation isn’t optional for methylation support – you need it.
Betaine sources:
- Beetroot
- Quinoa
- Spinach
- Sweet potato
What Often Gets In The Way:
Alcohol interferes with methylation. If you’re drinking regularly and wondering why your supplements aren’t working, this might be why. I’m not saying you need to quit entirely, but something to consider.
Chronic stress depletes B vitamins faster than you can supplement them. This is the hard truth: you can’t supplement your way out of a stress problem. The methylation support helps, but addressing the stress is essential.
Gut issues impact B vitamin absorption. If you have SIBO, dysbiosis, or low stomach acid, you might not be absorbing the nutrients from food or supplements effectively. This is worth investigating if you’re eating well and supplementing but still symptomatic.
When Methylation Support Isn’t Enough
Let me be clear: methylation support isn’t a magic bullet. If your symptoms continue despite proper supplementation and dietary support for several months, other factors are likely involved:
- Gut dysbiosis affecting nutrient absorption
- Chronic infections (like Epstein-Barr virus) depleting resources
- Heavy metal toxicity blocking methylation pathways
- Chronic inflammation from any source
- Hormonal imbalances that need direct attention
- Mitochondrial dysfunction (your energy factories aren’t working)
Sometimes methylation is the problem. Sometimes it’s a symptom of other problems. This is where comprehensive functional testing and clinical assessment become valuable.
The Honest Truth About Methylation
After years of working with this, here’s what I know:
Methylation support helps many people feel significantly better. But it’s not one-size-fits-all. Some people need high doses. Others need tiny amounts. Some do best with methylfolate. Others respond better to folinic acid (a different form).
The research gives us general principles, but individual response is where the real medicine happens. This is messy, nuanced work.
You might not have MTHFR variants and still have methylation issues. Or you might have the variants and feel fine. Genetics loads the gun; lifestyle and environment pull the trigger.
Start with diet and stress management. They’re free and they work. Then add targeted supplementation if needed. Test if it helps you make better decisions, or skip it if the clinical approach gives you answers.
And remember: feeling better doesn’t happen overnight. Give any changes at least 6-8 weeks before deciding they don’t work.